Anal Fissure
An anal fissure is a tear or ulcer in the lining of the anal canal, just inside the opening of your anus. They can be very painful, particularly when you are passing stools and for some time after. Anal fissures can also cause a small amount of bleeding, which you may notice in your stools, or on your toilet paper.
Anal fissures can be classified in several different ways. They can either be acute or chronic, depending on how long you have had the anal fissure. They can also either be primary or secondary, depending on the cause of your anal fissure. These classifications are outlined below.
- Acute anal fissure - is a fissure which has been present for less than six weeks
- Chronic anal fissure - is a fissure which has been present for six weeks, or more
- Primary anal fissure - is a fissure which has no identifiable underlying cause.
- Secondary anal fissure - is a fissure which is caused by an underlying condition.
How common are anal fissures?
Anal fissures are a common problem and can occur in both adults and children.
Symptoms
Anal fissures usually cause two main symptoms – pain and bleeding.
Pain
An anal fissure causes severe and sharp pain when you pass stools. Once this sharp pain has passed, it is normally replaced by a deep burning pain, which may be felt for several hours after you have been to the toilet.
Bleeding
Sometimes, an anal fissure can also cause bleeding when you pass stools. Most people notice a small amount of bright red blood, either in their stools, or on their toilet paper.
Causes
The cause of your anal fissure will depend on whether it is a primary or secondary fissure.
Primary anal fissures
This type of anal fissure is not caused by an underlying condition. However, it is thought to be associated with the way the muscles in your anus work.
The muscle which surrounds the anus (known as the internal sphincter) can sometimes contract too strongly (spasms). This causes increased pressure in the anal canal, making it more susceptible to tearing.
The increased pressure also restricts the blood flow to your anus. Reduced blood flow stops your body from being able to heal itself as well as normal, which means that it will be difficult for your fissure to heal naturally.
Secondary anal fissures
A secondary anal fissure is caused by an underlying condition. The conditions which can cause an anal fissure are outlined below.
Constipation
Constipation is the most common cause of a secondary anal fissure. Constipation is a very common condition which means that you are not passing stools as regularly as you normally do. This can cause your stools to become dry and hard.
Passing a hard stool can sometimes tear the lining of the anus. Avoiding passing stools because of the pain of an anal fissure will often worsen your constipation, which means that your fissure will not have a chance to heal.
Inflammatory bowel disease (IBD)
Inflammatory bowel disease (IBD) is a term that is used to refer to a number of conditions which cause inflammation in the intestines, such as Crohn’s disease and ulcerative colitis.
IBD can sometimes cause ulcers to form on the lining of the anus, which can lead to an anal fissure developing.
Sexually transmitted infection (STI)
If the lining of the anus becomes infected with an STI, it can cause the tissue to break down, resulting in an anal fissure.
Pregnancy
During the third trimester of pregnancy (week 29 to birth), your risk of having an anal fissure is increased. You may also develop an anal fissure during childbirth because the continual straining of your muscles can sometimes cause the lining of your anus to tear.
Cancer of the rectum
In very rare cases, an anal fissure can be a sign of cancer. Your GP will know if your fissure is a sign of a more serious illness from your other symptoms, and the appearance of your fissure. They will then be able to immediately refer you for further testing if they think it is necessary. However, it is important to remember that in the majority of cases, an anal fissure will not be caused by cancer.
Diagnosis
To diagnose an anal fissure, your GP will ask you about your symptoms and the type of pain you have been experiencing. They may also about your toilet habits.
Physical examination
In order to confirm a diagnosis of an anal fissure, your GP will usually have to carry out a physical examination. They will need to examine your anus by gently parting your buttocks. In most cases, your GP will be able to see a fissure.
However, if they cannot see any signs of a fissure, they may press gently on the edge of your anus. If you have a fissure, you will normally experience some pain when gentle pressure is applied.
Your GP should not need to perform a rectal examination (where they insert a lubricated, gloved finger into your anus to feel for abnormalities) in order to diagnose an anal fissure.
If your GP feels that something more serious may be causing your fissure, you will normally be referred to a specialist for a more thorough investigation. Which specialist you are referred to will depend on the suspected cause of your fissure.
Treatment
Like other small cuts or tears to the skin, an anal fissure will often heal by itself within a few weeks. However, you may require treatment to help ease the pain and discomfort that an anal fissure can cause.
It is important to see your GP if you have the symptoms of an anal fissure because it may be caused by an underlying condition. If this condition is not treated, your fissure may not be able to heal, and the problem will recur.
There are a number of treatments which can help encourage your anal fissure to heal, as well as easing your pain. These treatments are outlined below.
Softening stools
Because an anal fissure can make it very painful for you to pass stools, your GP will try and make the process easier for you by making sure your stools are soft. This will help you to pass them more easily, and with less pain and discomfort.
Some of the ways that your stools can be softened are outlined below.
Laxatives
To keep your stools soft, you will normally be prescribed a laxative, which is a type of medicine which helps make your stools easier to pass.
Adults with an anal fissure will normally be prescribed a bulk-forming laxative. Bulk-forming laxatives work by helping your stools to retain fluid, making them softer and denser.
Children with an anal fissure will normally be prescribed an osmotic laxative. This type of laxative works by increasing the amount of fluid in your bowels, which helps stimulate your body to pass stools.
Once you start taking your laxative, your GP may have to adjust the dose until you find that your stools are soft and easy to pass.
Fibre
As well as using laxative medication, you should also increase the amount of fibre you have in your diet. Foods that are high in fibre include:
- wholegrain bread, brown rice,pasta, oats, beans, peas, lentils, grains, seeds, fruit, and vegetables.
- Adults should be aiming to eat at least 18g of fibre a day. You can see how much fibre a food item contains by looking at the nutritional information on the back of the packet.
If you are increasing your intake of fibre, it is important to make sure you increase it gradually. A sudden increase can cause stomach cramps and make you produce more wind, leaving you feeling bloated. It is also important to make sure that you drink plenty of water. You should drink approximately 1.2 litres (6-8 glasses) of water a day, or more when exercising, or when it is hot.
Topical anaesthetics
A topical medicine is one which you apply directly to the affected area. Topical anaesthetics work by desensitising (numbing) the skin, helping to ease the sharp and severe pain that you may experience when passing stools.
The most commonly prescribed topical anaesthetic is lidocaine, which either comes in the form of a gel or an ointment. Lidocaine is usually used for between 1-2 weeks, as your fissure should start to heal by this time. It is normally applied shortly before you pass a stool, but you should always follow the instructions that come with the medicine.
 
Analgesics
If you experience prolonged, burning pain after passing stools, you may be prescribed an analgesic (painkiller), such as paracetamol, or ibuprofen.
Always follow the dosage instructions on the packet. Ibuprofen may not be suitable for people with asthma, or those with stomach, kidney, or liver problems. It is also not suitable for pregnant or breastfeeding women. Your GP, or pharmacist, will be able to advise you about what type of painkiller is best for you.
Diltiazem and nifedipine based creams
If your symptoms do not start to improve after a week, you may be prescribed a medicine called diltiazem or nifedipine. This type of medicine will help your anal fissure to heal, easing your symptoms of pain. It comes in the form of an ointment, and is applied directly to the anal area slightly inside usually every 12 hours.
GTN is not suitable for pregnant or breastfeeding women. It is also unsuitable for children. Headaches are a very common side effect of this type of medicine. Approximately 50% of people using GTN will experience a headache. Some people may also feel dizzy or light-headed after using GTN.
You will normally have to use GTN ointment for between 6-8 weeks, or until your fissure has completely healed.
Treating secondary anal fissures
If your anal fissure is being caused by an underlying condition, it is important that the condition is treated in order to help reduce the risk of your fissure recurring.
The treatment you receive will depend on what condition is causing your fissure. For example, if constipation is identified as the cause, you will usually be prescribed laxatives. STIs may have to be treated with a course of antibiotics.
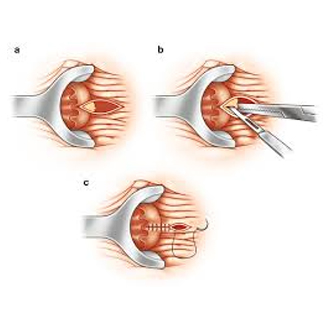
Referral
If your anal fissure is particularly severe, or does not respond to treatment after eight weeks, you may have to be referred to a colorectal surgeon. A colorectal surgeon is someone who specialises in surgery on either your colon (the main part of you large intestine) or rectum (the final section of your large intestine that ends with your anus). If your wound does not heal, it may require surgery to help prevent infection and ease your pain.
Prevention
It is not always possible to prevent an anal fissure from occurring. However, one of the best ways you can prevent a fissure from developing is to make sure you do not become constipated.
To prevent constipation, you should:
- eat plenty of fibre – at least 18g a day (see ‘treatment’ section),
- drink plenty of water – at least 1.2 litres (6-8 glasses a day), or more when you are exercising, or when it is hot,
- never ignore the urge to go to the toilet, and
- keep active – you should be doing at least 30 minutes of physical activity a day.
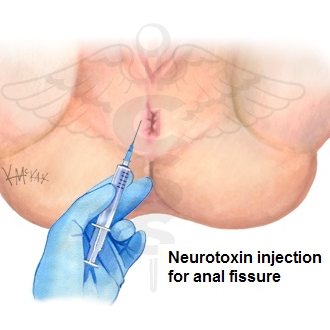
Patients who fail medical treatment or have recurrent fissures will require intervention
Treatment Options
We offer the best minimally invasive treatment for fissure as a day care surgery
Pudendal Block
All these procedures are accompanied by a pudendal block and a pain management protocol so that the patients have a relatively painless course of recovery and faster return to work.
The patient does not require any dressing or post op care