What symptoms do obstructed defaecation cause? The symptoms experienced include some or all of the following:
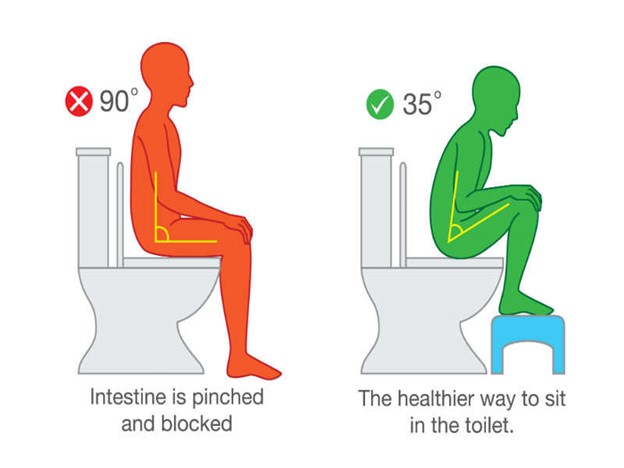
- Needing to strain
- Never feeling empty
- Frequent visits to the lavatory
- Fruitless visits to the lavatory
- Using a finger to help evacuation
As emptying may not be complete some patients describe leakage of a small amount of stool after they have been to the lavatory. How is obstructed defaecation investigated? Before confirming the diagnosis and finding a cause for obstructed defaecation, patients will require some form of endoscopic examination of the bowel either by flexible sigmoidoscopy or colonoscopy to ensure that it is otherwise healthy.
The most useful test to determine the cause of obstructed defaecation is a video proctogram. This gives information not only about structural problems but also whether or not the pelvic floor works properly. A transit study is often performed to establish Most patients will also have tests of their sphincter muscle function (anorectal physiology) and an endoanal ultrasound scan to look for any damage to the muscle.
How is obstructed defaecation treated?
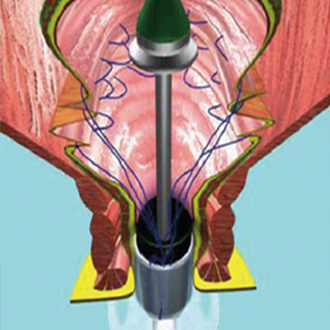
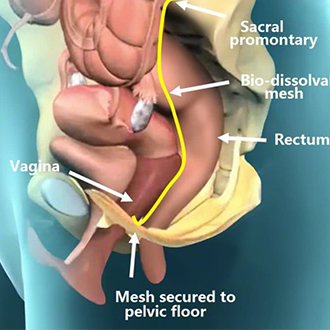
Keeping the stools soft, avoiding straining and the use of glycerine suppositories will help many patients. Where the problem is due to function then biofeedback / physiotherapy is usually recommended to enable patients to regain co-ordination of their pelvic floor. If a physical cause for the symptoms is found surgical correction may be recommended. Such procedures might include rectocele repair, or ventral mesh rectopexy for patients with enterocele or internal prolapse